It’s a persistent image in popular culture and often in casual conversation: IVF and twins. Many people mistakenly believe that in-vitro fertilization almost invariably leads to twin or multiple pregnancies. While it’s true that the incidence of twins was historically higher with IVF, and such stories are certainly memorable, this perception largely stems from outdated practices and a skewed memory bias. The reality today, driven by advancements in reproductive medicine and a commitment to patient safety, tells a different story.
One significant reason for the misconception is the “memorability factor.” Twin pregnancies, especially after a long and arduous journey through infertility, are naturally more striking and talked about than singleton births. These joyful, often miraculous outcomes stand out in people’s minds, while the far more common singleton IVF pregnancies often go unremarked upon, or the fact that IVF was even involved remains private.
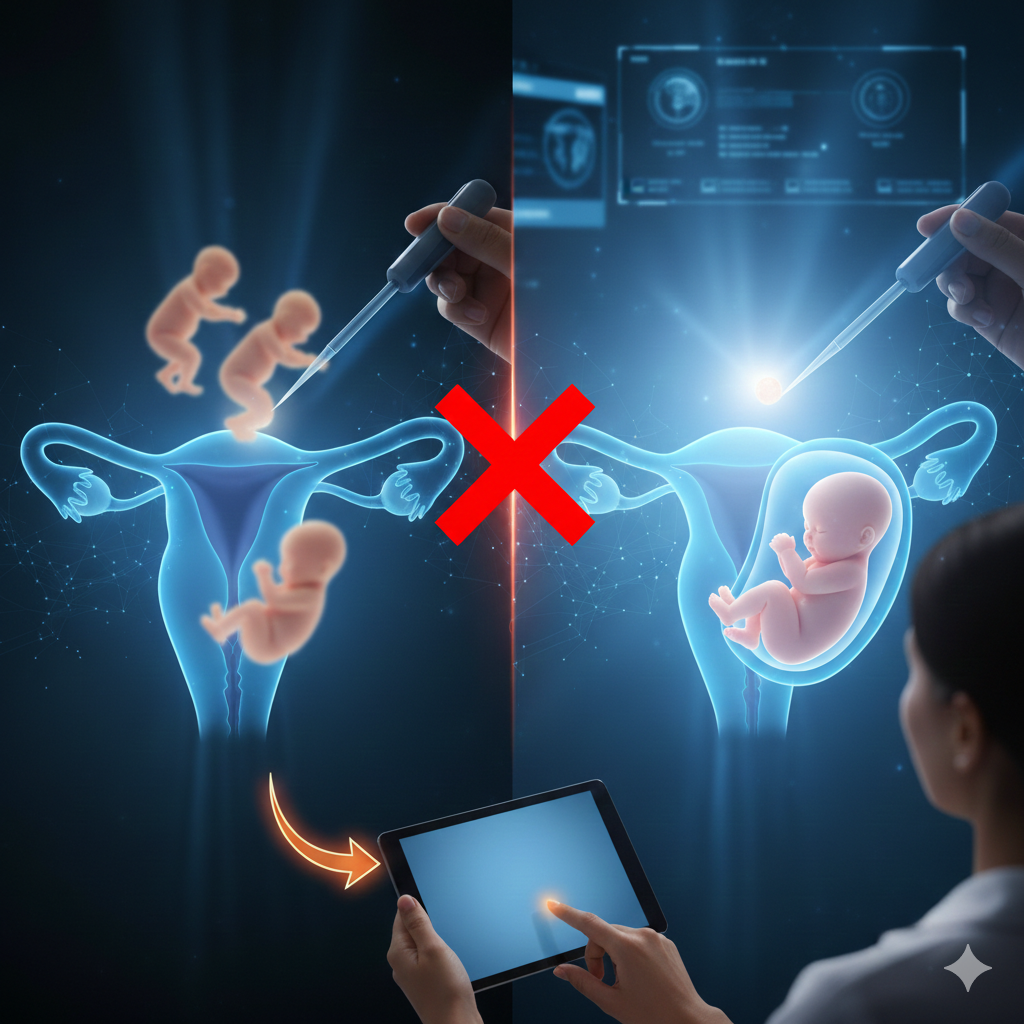
However, the primary driver of past multiple pregnancies in IVF was a practice born out of necessity: the transfer of multiple embryos. In earlier days, IVF success rates were considerably lower. To compensate and increase the odds of a successful pregnancy, clinics would often transfer two, three, or even more embryos into the uterus at one time. The logic was simple: if more embryos were transferred, at least one might implant. The unintended consequence, however, was a higher rate of multiple gestations when several embryos successfully implanted.
While the idea of an “instant family” with twins might seem appealing to couples struggling with infertility, it’s crucial to understand the medical implications. Twin pregnancies, and even more so higher-order multiple pregnancies (triplets or more), carry significantly increased risks for both the mother and the babies. These risks include premature birth, low birth weight, pre-eclampsia, gestational diabetes, and a higher chance of complications during delivery.
Recognizing these risks, the global best practice in modern IVF has shifted dramatically. With significant improvements in laboratory techniques, embryo selection, and cryopreservation (freezing), the focus is now firmly on achieving a healthy singleton pregnancy. This means transferring only a single, high-quality blastocyst (an embryo that has developed for five to six days) at a time, and freezing any other viable embryos for future use. This approach, known as elective single embryo transfer (eSET), maximizes the chance of a healthy pregnancy while minimizing the risks associated with multiples.
Therefore, while the image of IVF twins might linger in the public consciousness, it’s an increasingly outdated one. Modern IVF aims for one healthy baby at a time, reflecting a commitment to the safest and most successful outcomes for families.
For accurate information on current IVF practices and to understand your treatment options, visit https://www.drmalpani.com/knowledge-center