In the world of In Vitro Fertilization (IVF), there is a quiet but fierce debate happening behind the laboratory doors: When is the best time to transfer an embryo?
While science increasingly points toward the Blastocyst (Day 5) stage as the gold standard, many clinics still insist on transferring embryos on Day 3. For the frustrated patient, this feels less like medical intuition and more like a lack of confidence in the laboratory’s technical competence.
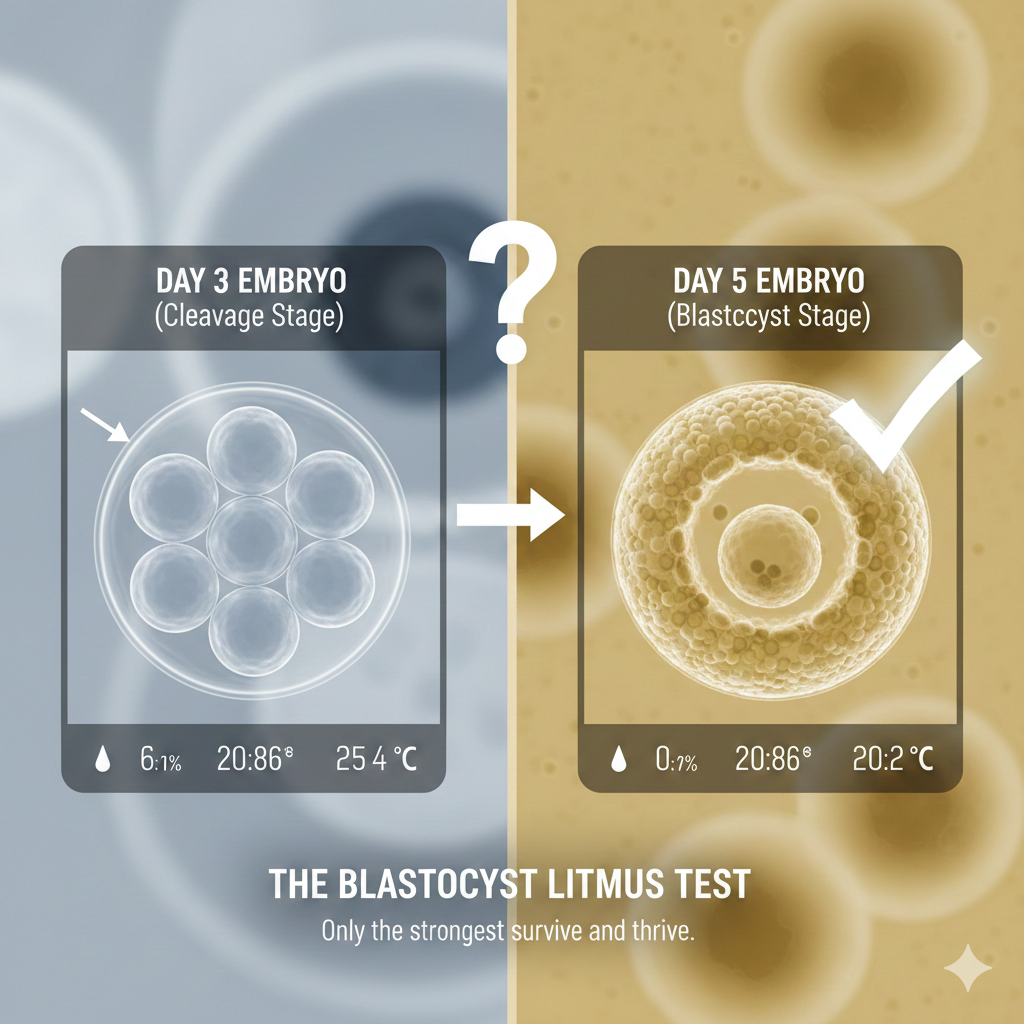
The Biological Reality: The “Blastocyst Litmus Test”
To understand the frustration, we have to look at the math of human development. A Day 3 embryo (cleavage stage) is a collection of about 6–8 cells. A Day 5 embryo (blastocyst) has expanded to nearly 100 cells and has begun to differentiate into what will become the baby and the placenta.
Why the Reluctance? The “Zero Transfer” Fear
If Day 5 is more “natural” for implantation, why do so many clinics push for Day 3? The answer often lies in risk management—not for the patient, but for the clinic.
-
Avoiding the “Empty Handed” Conversation: If a lab attempts to grow ten embryos to Day 5 and none survive, they have to tell the patient there will be no transfer. This is a devastating conversation.
-
Shifting the Blame: By transferring on Day 3, the clinic “completes” the procedure. If the pregnancy fails, they can attribute it to “implantation failure,” “bad luck,” or “poor egg quality.” It protects the clinic from taking personal responsibility for a sub-optimal laboratory environment.
-
Technical Limitations: Maintaining a stable environment (pH levels, temperature, air quality) for five days is significantly harder than for three. A Day 3 transfer is often a red flag that a lab may not have the high-level equipment or the highly skilled embryologists required for long-term culture.
The Lab vs. The Uterus: The Great Myth
Many doctors argue that the “maternal environment is the best incubator.” While the uterus is indeed a miracle of nature, modern IVF incubators are designed to mimic those conditions precisely.
The Hard Truth: If an embryo is healthy enough to become a blastocyst in the uterus, a high-quality IVF lab should be able to achieve the same result. If the embryo “dies” in the lab on Day 4, it was almost certainly going to stop developing in the uterus as well.
The lab doesn’t kill the embryo; it simply provides a transparent window into its viability.
Why You Should Insist on Day 5
Insisting on a Day 5 transfer isn’t just about being picky; it’s about efficiency and emotional protection.
-
Natural Selection: Roughly 50% of embryos that look perfect on Day 3 stop growing by Day 5 due to genetic abnormalities. A Day 5 transfer prevents you from undergoing the physical and emotional toll of transferring an embryo that never had a chance.
-
Higher Success Rates: Because you are only transferring the “survivors,” the pregnancy rate per transfer is significantly higher.
-
Accountability: It forces the IVF clinic to maintain the highest standards of technical competence.
If a clinic is hesitant to grow embryos to Day 5, it’s time to ask the hard questions. A confident embryologist shouldn’t fear the “Day 5 drop-off.” They should embrace it as the most honest way to give their patients the best possible chance at a healthy baby.
Still Confused ! You can get answers from Dr. Malpani instantly at https://www.drmalpani.com/chat-w-chatbot/index.html